
HIP DISLOCATION
Hip dislocations found in children are either congenital or traumatic. Congenital hip dislocation (CHD) is a condition in which a child is born with an unsteady hip. Traumatic is the result of an accident or large force that causes a hip to dislocate.
If your child needs surgery or casting, our Fracture Care Clinic opens every day and you do not need an appointment. Surgery rooms get scheduled every morning, so your child receives the care and attention they need right away.
Hip Dislocation
 Hip dislocations found in children are either congenital or traumatic. Congenital dislocation of the hip is the result of dysplasia of the femoral head or acetabulum. Congenital hip dislocation (CHD) is a condition in which a child is born with an unsteady hip. It’s the result of abnormal formation of the hip joint that happens during the early stages of fetal development. This condition is also known as “developmental dysplasia of the hip.” And as your child grows, this instability worsens.
Hip dislocations found in children are either congenital or traumatic. Congenital dislocation of the hip is the result of dysplasia of the femoral head or acetabulum. Congenital hip dislocation (CHD) is a condition in which a child is born with an unsteady hip. It’s the result of abnormal formation of the hip joint that happens during the early stages of fetal development. This condition is also known as “developmental dysplasia of the hip.” And as your child grows, this instability worsens.
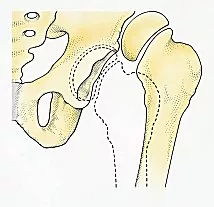
In the child’s hip, the ball-and-socket joint may sometimes dislocate. Clearly, this means that with movement, the ball will slip out of the socket. Sometimes, the joint may even dislocate completely.
On the other hand, Traumatic hip dislocation is an orthopedic emergency. Certainly, large forces are necessary to cause a hip dislocation like this. As a result, other injuries may have occurred including severe injuries and fractures. Even though Hip Dislocation is painful, proper and fast diagnosis and the right medical management can reduce suffering.
The doctors at Medical City Children’s Orthopedics and Spine Specialists are highly skilled and experts at diagnosing and treating hip disorders.
CHD Cause
In many cases, the cause of CHD is unknown. The contributing factors are low levels of amniotic fluid in the womb and breech presentation in which your baby is born hips first. While there might be a family history of the condition, confinement in the uterus may cause CHD. That is why a baby is more likely to have this condition if a woman is pregnant for the first time. It is because here the uterus hasn’t been stretched previously.
Risk Factor
Even though any infant can have the condition, CHD is more common in girls than in boys. A doctor routinely checks your newborn for any signs of hip dislocation. During their first year of life, experts also keep examining your child’s hips.
Traumatic Hip Dislocation
The most common cause of this type of hip dislocation is direct trauma, especially road traffic accidents and falls.
- Children may sustain hip dislocation even from minor trauma.
- Traumatic hip dislocations are often the result of motor vehicle accidents or significant falls from height.
- People often easily overlook hip dislocations if there is a related femur fracture.
- Experts need to manage and reduce hip dislocations in children gently to avoid injury to the femoral epiphysis.
- Traumatic dislocations may be of three types: posterior, anterior, or central.
Posterior Dislocation of The Hip
This occurs because of a major force to a flexed knee and hip. This can also cause other serious injuries such as fractures of the posterior acetabular or femur. Doctors usually make the diagnosis with an AP X-ray.
Anterior Dislocation of the Hip
This injury is less common. It causes pain in the hip and causes an inability to walk or move the leg. The leg rotates externally, abducts, and extends at the hip. The initial treatment is to provide analgesia, the reduction under general anesthetic, etc.
QUESTIONS AND ANSWERS
What causes hip dislocation in children?
Hip dislocation in children can occur due to various causes, including:
- Congenital Hip Dysplasia: This refers to a common cause, where the hip joint doesn’t develop properly, making it prone to dislocation.
- Trauma: A direct blow or forceful impact to the hip region, such as in a car accident or a fall, can dislocate the hip.
- Developmental Issues: Conditions like cerebral palsy or muscular dystrophy can lead to muscle imbalances that may contribute to hip dislocation.
- Genetic Factors: Some children may have a genetic predisposition to hip instability or dislocation.
How do doctors diagnose and treat hip dislocation in children?
Diagnosis and treatment of hip dislocation in children involve the following steps:
- Clinical Examination: A healthcare provider will perform a physical examination, looking for signs of hip instability, asymmetry, and limited range of motion.
- Imaging: X-rays are typically used to confirm the diagnosis and assess the severity of the dislocation. Ultrasound may be used in infants to evaluate hip dysplasia.
- Treatment: The treatment approach depends on the cause and severity of the dislocation:
- Non-Surgical Methods: In some cases, especially with congenital hip dysplasia, non-surgical methods like the use of a Pavlik harness or a spica cast may be effective in repositioning the hip joint.
- Closed Reduction: If the hip becomes dislocated, but the bones are still aligned, a closed reduction procedure may be performed to manipulate the joint back into its proper position under anesthesia.
- Surgery: Doctors recommend surgical intervention for severe hip dislocations or when conservative methods fail. Surgical procedures may involve open reduction, osteotomies, or other techniques to stabilize the hip joint.
- Rehabilitation: After treatment, rehabilitation and physical therapy are essential to help the child regain hip joint function and prevent recurrence.
What are the potential complications and long-term effects of hip dislocation in children?
Hip dislocation can lead to various complications and long-term effects, including:
- Chronic Pain: Untreated or improperly managed hip dislocations can result in chronic pain and discomfort.
- Gait Abnormalities: Hip instability and dislocation can affect a child’s walking pattern and may lead to long-term gait abnormalities.
- Early-Onset Arthritis: Hip dislocation can increase the risk of developing early-onset hip arthritis in adulthood.
- Functional Limitations: Depending on the severity and treatment success, some children may experience long-term functional limitations or mobility challenges.
- Hip Dysplasia: Hip dysplasia may persist or develop as a consequence of hip dislocation, requiring ongoing monitoring and treatment.
Early diagnosis and appropriate treatment are crucial to minimize complications and optimize outcomes for children with hip dislocation. Timely intervention can help ensure the best possible hip joint function and quality of life.
Central Dislocation of the Hip
This condition happens when a fall or force is put along the length of the femur, and the head of the femur drives through the fractured acetabular floor. The level of leg deformity depends on the extent and nature of penetration into the pelvis. The leg shortens, abducts, or adducts, and rotates internally or externally. For diagnosis, our doctors usually use an AP pelvic X-ray.
CHD Symptoms
CHD may have no symptoms. That is why specialists will routinely test your child for the condition. If your child has this condition, the common symptoms are:
- Legs that turn outward or seem different in length
- Restricted motion
- Folds on the legs and buttocks that appear uneven when the legs extend
- Delayed development of gross motor, which impacts the way your child sits, crawls, and walks
Diagnosis
Screening for CHD generally happens at birth and also occurs throughout the first year of your child’s life. Furthermore, a physical exam is the most common screening method. Hence, the doctor will gently move and check your child’s hip and legs to look for any clicking or clunking sounds. Such a sound may indicate a dislocation. This exam comprises two tests:
- Ortolani test – During this test your child’s orthopedic doctor will apply upward force to move your child’s hip away from the body. The movement away from the body is abduction.
- Barlow test – In this test, your child’s doctor will apply a downward force to move your child’s hip across the body. Applying force toward the body is adduction.
These tests are only appropriate before your child is 3 months old. In older babies and children, findings that help indicate CHD are: limited abduction, limping, and different leg lengths if a single hip is affected.
Imaging tests can help confirm a CHD diagnosis. Doctors check ultrasounds for babies who are younger than 6 months old. They utilize X-rays for examining older babies and children.
Treatment
If your baby, younger than 6 months of age, has CHD, it is quite likely that the child will fit for a Pavlik harness. This harness helps press the hip joints into the sockets. The harness plays a crucial role in abducting the hip by securing the legs in a frog-like posture. Depending on the age of the child and the severity of the condition, your baby may have to wear this harness for 6 to 12 weeks full-time or part-time.
If the treatment with a Pavlik harness seems to be unsuccessful, or your baby is too big to fit in the harness, surgery might be necessary. Subsequently, surgeons perform the procedure under general anesthesia. Sometimes, this may involve simply maneuvering their hip into the socket. This procedure is called a closed reduction.
Also, the surgeon may surgically lengthen the tendons of your baby and eliminate other obstacles before repositioning the hip. This procedure is called an open reduction. After repositioning your baby’s hip, their hips and legs will be in casts for at least 3 months. However, if your child hasn’t responded well to treatment or is 18 months or older, he may need femoral or pelvic osteotomies to reposition the hip. In this method, a surgeon will reshape or divide the acetabulum of the pelvis (the hip socket) or the head of the femur (the ball of the hip joint).
Prevention
Unfortunately, CHD cannot be prevented. It’s crucial to take your child with this condition to regular checkups. This is how the doctors can identify and treat the condition ASAP.
The long-term outlook
When the doctor identifies CHD earlier and your baby gets treatment with a Pavlik harness at the right time, complicated invasive treatment is not likely to be necessary. According to the experts, around 80 and 95 percent of cases that are identified early get successful treatment. And the treatment is determined by the seriousness of the condition.
The success rate might vary from one surgical treatment to another. While some treatments only require one procedure, others may need multiple surgeries and years of proper monitoring. If your child’s CHD does not get proper treatment in early childhood, it can lead to early arthritis and severe pain in the future. And in serious cases, even total hip replacement surgery might be necessary. Even if your child’s CHD treatment is successful, they must keep visiting an orthopedic specialist regularly to ensure the problem doesn’t come back and that their hip continues to grow properly.
Conclusion
When it comes to treating congenital and traumatic hip dislocations, the sooner the diagnosis, the better. Consulting trusted orthopedic doctors like those at the Medical City Children’s Orthopedics and Spine Specialists will help you properly diagnose the condition and get the best treatment accordingly. To make it convenient for our patients, we have offices in Arlington, Dallas, Flower Mound, Frisco, and McKinney, TX. Finally, we are accepting new patients and invite parents to give us a call and make an appointment.
___________________
Footnote:
The Royal Children’s Hospital: Hip Dislocation
Call 214-556-0590 to make an appointment.
Comprehensive services for children from birth through adolescence at five convenient locations: Arlington, Dallas, Flower Mound, Frisco and McKinney.
