
PARS DEFECT
A Pars Defect or spondylolysis is a stress fracture of the bones of the lower spine. These fractures typically occur due to overuse. They can be on one or both sides of the vertebrae. It is a common cause of low back pain in children and adolescents.
At Medical City Children’s Orthopedics and Spine Specialists, our expert Pars Defect Doctors are dedicated to diagnosing and treating spinal problems in children and ensuring comprehensive care tailored to each patient’s needs. With advanced techniques and a compassionate approach, our team is here to diagnose, treat and care for children suffering from Pars defect.
If your child needs surgery or casting, our Fracture Care Clinic opens every day and you do not need an appointment. Surgery rooms get scheduled every morning, so your child receives the care and attention they need right away.
Pars Defect
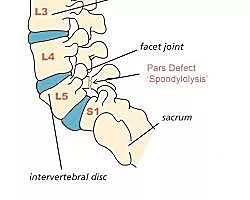 Pars defect, also known as Spondylolysis, affects a tiny spinal bone, namely pars interarticularis, found in children. It happens from a small problem in the spine, like a small fracture or crack between two vertebrae (spine bones). This spine condition causes back pain that can be painful enough. However, the Pars defect is treatable without any surgery in most cases! So, consult your doctor for treatments whenever you see your kids with back pain.
Pars defect, also known as Spondylolysis, affects a tiny spinal bone, namely pars interarticularis, found in children. It happens from a small problem in the spine, like a small fracture or crack between two vertebrae (spine bones). This spine condition causes back pain that can be painful enough. However, the Pars defect is treatable without any surgery in most cases! So, consult your doctor for treatments whenever you see your kids with back pain.
Generally, a Pars defect or Spondylolysis is a spine condition where the problem lies between the connection of vertebrae to what the spine is made of. Ignoring this condition in your children may cause small cracks and spine fractures, especially after repeated injuries while participating in any sports. However, research shows that treatments are successful if you take your child to a doctor and begin the therapies and medication early.
Why You Should See a Spine Specialist for a Pars Defect
When it comes to diagnosing and managing a Pars defect, getting help from a spine specialist makes all the difference. Because this condition affects a very small but important part of the spine, it can sometimes be tricky to spot and manage without expert guidance. Specialists—including pediatric orthopedic surgeons, physical therapists, and radiologists—are trained to look for subtle clues, use advanced imaging like MRI or CT scans, and develop a treatment plan built just for your child.
Here’s why professional assessment matters:
- Accurate Diagnosis: A spine specialist ensures your child gets the right diagnosis, catching small fractures or subtle injuries that can be missed.
- Customized Treatment: Each child’s activity level, age, and symptoms are unique. Specialists tailor therapies—ranging from rest and bracing to physical therapy—so your child gets the safest and quickest recovery.
- Early Intervention: The sooner a Pars defect is identified and treated, the better the outcome. Starting the correct treatments early helps prevent worsening cracks or further complications.
- Team-Based Care: Managing spinal conditions often means working together with physical therapists and radiologists, providing comprehensive care all under one roof.
So, if your child has persistent back pain—especially after sports or sudden movements—don’t wait. A visit to an experienced spine specialist gives your family peace of mind, a clear diagnosis, and a plan designed for a strong, healthy recovery.
QUESTIONS AND ANSWERS
What is a Pars defect, and what caused it in my child?
A Pars defect is a condition characterized by a stress fracture or defect in a specific part of the vertebra known as the pars interarticularis. This condition is commonly seen in the lower spine, typically in the lumbar region. Pars defects can result from overuse, repetitive stress on the spine, or may have a genetic component. The doctor will explain the condition and its potential causes, taking into account the specific case of your child.
What are the treatment options for my child's Pars defect?
The treatment for a Pars defect can vary depending on the severity of the condition and the child’s symptoms. Treatment options may include rest, physical therapy, bracing, or in some cases, surgical intervention. Recovery time can also vary but may take several weeks to months, with the potential for full recovery. The doctor will discuss the specific treatment plan and provide an estimated timeline for healing.
Will my child fully recover, and can they return to physical activities?
Many children with Pars defects can return to sports and physical activities after appropriate treatment and rehabilitation. However, precautions may be necessary to reduce the risk of future injuries. The doctor can provide guidance on a safe return to sports, recommend injury prevention strategies, and discuss any necessary precautions, such as proper warm-up techniques, activity modification, and exercises to strengthen the supporting muscles of the spine.
For the very best spine doctors, Schedule an Appointment for your child to be seen by one of the doctors or surgeons at the Medical City Children’s Orthopedic and Spine Specialists
How Common Is a Pars Defect?
Medical research reveals that almost 3% to 7% of Americans, especially children and teens who attend sports like football and gymnastics, are affected by a Pars defect. As mentioned earlier, spondylolysis occurs due to small fractures or cracks in the spine bones, such as those between two vertebrae. For example, children overextend or overstretch their spines participating in such games, but do not bend inward. It causes slight cracks in the vertebrae!
Spondylolysis and Spondylolisthesis
These terms may sound similar and even relate to each other, but not the same. Spondylolisthesis occurs when one spine body or vertebra slips out of its place over another below. Moreover, it results in Spondylolysis (Pars defect) because the small cracks or fractures between the connection of two vertebrae can make the bone slip.
Pars Defect Causes
When your child has Spondylolysis, a specific section in the vertebra in the spine, known as the pars interarticularis, may be weak. It is a thin piece of spinal bone that connects the vertebrae below and above to create a properly working spine while ensuring its movement. And when it cracks, it is called a pars defect. However, there is no certain reason behind it. It may be that your child is born with thin vertebrae, which increases the risk of Spondylolysis.
Also, a Pars defect may be a problem in your gene that plays a great role in this case. In addition, repetitive injuries to the lower back of your children when they participate in sports or any other intense activities can weaken the tiny bone, pars interarticularis. Gradually, a Pars defect can occur.
Pars Defect Symptoms
Sometimes, your child may not feel any symptoms, like back pain, even while having it. Lower back pain is the most common and prime symptom of a Pars defect. However, the pain may feel different than usual, which you should ask your kids to notice. Such as
- Feeling like muscle strains
- It gets worse as the lower back pain extends
- Spreading across the lower back
Furthermore, the pars defect symptoms can arise even after teenage growth, although the cracks appear in childhood. That’s why the typical age of diagnosis for Spondylolysis is at the age of fifteen or sixteen, but younger in girls.
Pars Defect Complications
If you overlook Spondylolysis and delay in treatment, the condition worsens and leads to Spondylolisthesis. Moreover, your children can experience severe pain when the vertebra presses on the nerve around it. Therefore, you may need to take your kids for surgery to relieve these symptoms and return to a normal life. In addition, your child may find it difficult to move and lose muscle flexibility. So, getting the treatments may help them get over it.
Diagnosis
To diagnose the condition of a Pars defect in your children, your doctors may ask about the symptoms they feel and their medical history. Also, you can expect your healthcare provider to give a few imaging tests to your kids, like:
- CT or MRI scans to identify the small cracks or fractures and figure out their spine conditions, like a pinched nerve or herniated disc, to determine whether it can lead to back pain in the future.
- X-ray of your child’s lower back to see whether there are any cracked vertebrae
Pars Defect Treatments
Most healthcare providers suggest nonsurgical options to treat Spondylolysis. Pars defect treatments generally include physical therapy and medications. Early treatment reduces pain and allows the cracks to heal while ensuring your kids can return to regular activities quickly. But for complete relief, make sure your children follow the regimen recommended by doctors. The timeline can be for a few weeks or a few months, depending on the severity of the condition. However, here are some nonsurgical treatments available for Pars defects:
Medications:
Doctors often recommend nonsteroidal anti-inflammatory drugs to reduce inflammation and low back pain. If required, the health care provider can suggest even stronger medication based on the condition of the pars interarticularis.
Physical therapy:
If you begin physical therapy for your children early, Spondylolysis may be treated. A physical therapist can recommend exercises to improve spine flexibility and strengthen the muscles around it. Therefore, your kids can feel free to move without pain.
Bracing:
Doctors suggest that many children wear a back brace to reduce the pain and heal the fracture while stabilizing their spine. Moreover, they advise kids to take a break from intense physical activities, especially sports!
Steroid injections:
This one is another alternative to relieve pain. Injecting steroids in the affected area of the lower back can give quick pain relief. But since they are children, it is better to avoid steroid medication!
Surgery for a Pars Defect
Surgery is rarely needed to treat a pars defect. Most children improve with early nonsurgical treatments mentioned earlier. However, doctors may recommend surgery to stabilize the spine and help manage the fracture. Spinal fusion isn’t always necessary to connect vertebrae and create one solid bone.
Surgeons remove damaged tissue and stabilize the fracture using bone from another part of the body. This helps your child return to normal and perform daily activities again. If direct repair isn’t possible, such as with significant vertebral slippage, spinal fusion might be recommended. Fusion joins the affected vertebrae, so they move as one unit. This procedure may be done from the back, front, or both approaches. Surgeons might use rods and screws to stabilize the spine while the bones heal.
Surgery is usually considered only after trying all nonsurgical treatments. Your doctor will guide you in choosing the best approach for your child.
Direct Repair Techniques
Doctors may suggest a direct repair of the pars defect, especially in children and teenagers. A common technique is Buck’s fusion, which uses a screw to connect both sides of the fracture. This method stabilizes the bone while preserving the spine’s natural flexibility and motion.
Unlike traditional fusion, it allows movement in the affected part of the spine.
The best option depends on the defect’s severity and location, plus your child’s age and activity level. Surgery is considered only when pain or instability continues after trying nonsurgical methods.
Interbody Fusion: When Is It Considered?
Interbody fusion is sometimes considered when vertebral slippage is significant or other treatments have failed. In this procedure, the surgeon removes the damaged disc between two vertebrae. They insert a small spacer or cage to maintain proper spacing and support the vertebrae.
Bone eventually grows around the spacer, fusing the vertebrae and stabilizing the spine.
This method prevents unwanted movement and helps relieve pain or nerve symptoms. It is typically reserved for more serious cases of pars defect. Interbody fusion is not the first treatment option. Most children with pars defects do well with nonsurgical treatments. Surgery is only recommended when necessary.
Decompression Surgery: When Is It Needed?
If the pars defect or spondylolisthesis compresses nerves and causes pain, doctors may consider decompression surgery. This surgery, called a laminectomy, relieves nerve pressure and reduces symptoms like pain, numbness, or weakness. Decompression is rarely required and is only considered after nonsurgical methods fail. It becomes an option when nerve symptoms significantly impact daily life. Your healthcare team will evaluate all options to ensure the best outcome.
Minimally Invasive Options for Pars Defect
Doctors sometimes recommend minimally invasive spine surgery when nonsurgical methods aren’t effective. These surgeries involve smaller incisions than traditional procedures and usually result in less pain. Smaller cuts mean lower infection risk and faster recovery for your child.
Surgeons use special tools and imaging to reach the area while avoiding surrounding tissues. This method stabilizes the spine and repairs the fracture with less disruption. Minimally invasive techniques help children return to normal activities sooner. Talk to your healthcare provider to see if this is right for your child’s condition.
Post-Surgical Care After Pars Defect Surgery
After your child undergoes surgery for a pars defect, careful follow-up and post-surgical care are essential for a smooth recovery. In the initial days, your little one might experience some discomfort around the surgical site—doctors typically manage this with a combination of pain relief medications such as anti-inflammatories and, in some cases, mild analgesics. The use of stronger medications like opioids is generally minimized for children due to risks of dependence and side effects.
During the recovery process, doctors may recommend some activity restrictions for your child to give their spine the best chance to heal. This usually means they should avoid heavy lifting, bending, or twisting for several weeks or months—think of it as a medical “pause button” on any rough-and-tumble adventures or sports. Some children may also be given a back brace for extra support and stabilization during the early healing period.
Follow Up Doctors’ Appointments
Regular follow-up appointments are a vital part of the recovery journey. At these visits, the surgeon will check in on healing progress, make sure the spine is stabilizing well, and look out for any red flags. Imaging tests like X-rays might be ordered to ensure everything is right where it should be. Once your child is on the mend, physical therapy will often be added to the mix. Under the guidance of a pediatric physical therapist, your child will work through gentle exercises to boost flexibility, rebuild strength in their back and core, and gradually improve movement without pain.
It’s also important to keep an eye out for any warning signs between visits. If your child develops sudden or severe pain, numbness, weakness, fever, chills, or any unusual drainage from the surgical area, contact your healthcare provider right away. For long-term spine health after surgery, encourage your child to maintain a healthy weight and protect their back during everyday activities. Supporting them through a safe recovery now helps set them up for an active, pain-free future.
Role of Physical Therapy
Physical therapy plays a crucial role in recovery. A physical therapist will carefully introduce exercises designed to rebuild core and back strength, improve flexibility, and encourage good posture. Starting therapy at the right time helps your child regain movement and confidently return to normal activities when ready.
Regular Follow-Ups and Monitoring
During the healing process, regular check-ups with your child’s surgeon are essential. These visits allow the doctor to track recovery, ensure the surgical site is healing properly, and may include imaging tests such as X-rays to check for proper bone growth and placement.
What to Watch For
Be alert for any unusual symptoms during recovery. If your child experiences increased pain, new nerve symptoms (like numbness or weakness), fever, chills, or any unusual drainage from the surgical site, contact your healthcare provider right away. Early attention to these signs can help prevent complications.
Long-Term Spine Health
Finally, encourage healthy habits moving forward. This includes maintaining a balanced weight, staying active at an appropriate level, practicing good posture, and, if relevant, avoiding smoking, as it can interfere with bone healing. With attentive post-surgical care and guidance from your healthcare team, most children can look forward to a strong and healthy recovery after surgery for a pars defect.
Post-Surgery Precautions and Activity Limitations
After a surgery to repair a pars defect, your child will need to follow certain precautions to ensure the best possible recovery. Doctors typically recommend avoiding activities that involve excessive bending, lifting, or twisting for several weeks to months. These restrictions are necessary to protect the healing site and prevent any additional stress on the spine. In some cases, your healthcare provider may prescribe a back brace to give extra support and stability, especially during the early phases of recovery. The brace helps limit movement, giving the bones and tissues time to mend properly.
During this period:
- Encourage your child to rest and avoid high-impact sports or rough play.
- Follow all guidelines provided by your child’s doctor or physical therapist regarding safe movements and exercises.
- Attend recommended physical therapy sessions to gradually reintroduce movement and rebuild strength.
By sticking closely to these precautions and working with the medical team, you’ll help your child achieve the best outcome and get them back to their routine safely.
Potential Post-Surgical Complications to Watch For
Even after a successful surgery for a pars defect, it’s important to stay vigilant and monitor for any signs of trouble during your child’s recovery. While routine follow-up visits and imaging will help your doctor keep an eye on the healing process, there are certain symptoms you and your child should watch for at home:
- Sudden or Severe Pain: Although some discomfort is normal after surgery, increasing pain—or pain that’s different from what’s expected—should not be ignored.
- New Numbness or Weakness: If your child experiences tingling, numbness, weakness, or difficulty moving their legs, contact the doctor right away.
- Signs of Infection: Keep an eye out for fever, chills, redness, unusual swelling, or drainage from the surgical site.
- Changes in Bladder or Bowel Control: Trouble going to the bathroom or a loss of control can be signs that nerves are affected and require immediate medical attention.
Encourage your child not to “tough it out” if something feels off. It’s always better to check with your healthcare provider, especially during the early stages of healing. If any of these symptoms develop, seek prompt medical attention to ensure your child stays on the healthiest track possible.
Role of Physical Therapy After Surgery
After your child starts to heal from surgery for a Pars defect, physical therapy becomes a crucial step in their recovery process. A licensed physical therapist will create a tailored plan filled with gentle stretches and strengthening exercises focused on the back and abdominal muscles. These exercises help restore flexibility, improve core strength, and support proper posture, which all work together to protect the spine and prevent future injuries.
Physical therapy doesn’t just rebuild muscle; it helps your child regain confidence in their movement by teaching the safest ways to bend, walk, and return to daily routines. This guidance encourages steady progress while reducing the risk of setbacks, so your child can get back to their favorite activities sooner and with less discomfort. With close supervision from both your healthcare provider and the physical therapist, recovery can be both safe and effective.
Prevention
There is no way to prevent a Pars defect. Yes, you can reduce the risks of fracturing bones. For example, if you see your children with low back pain and interfering with their daily activities, consult a doctor first to start the treatments and medications as early as possible. It will give your kids a better outcome and lessen the need for surgery in the future. Also, physical therapy will strengthen the back and abdominal muscles, which enhances lower back support. Moreover, allow your children’s activities, like swimming, to lower the risks of cracks when they have Spondylolysis because it will be gentle on your back.
Timeline for Recovery from Pars Defect
The sooner your kids start treating their Parsonage-Turner syndrome, the faster they will return to regular activities. But it can take a few weeks or even a few months to get back your spine flexibility and mobility. The recovery time varies for every individual based on the condition.
When You Should Take Your Child to a Healthcare Provider
The nonsurgical treatments for Spondylolysis are more effective when one starts them at an earlier stage. Therefore, you should see your children to a doctor ASAP whenever you see them experiencing low back pain and its interference with common activities in life.
Final Thoughts
A pars defect can cause severe lower back pain in your child if you leave it untreated. Additionally, it can disrupt their daily activities. While treating early with physical therapy and medications, your kids can get relief from pain without surgery. Moreover, you can encourage your children to undertake strengthening workouts to ensure strong stomach and back muscles to reduce the chances of back injuries and prevent Spondylolysis from coming back. Also, consult with doctors to learn about different activities to reduce Spondylolysis complications.
In addition to targeted exercises, consider a few lifestyle adjustments for better long-term spine health. Maintaining a healthy weight eases pressure on the spine and reduces the risk of further injury. If your child is older and participates in activities where smoking might be a concern, remind them that smoking can impede bone healing and increase the risk of complications. Finally, teaching your child to use proper posture and ergonomic techniques—like lifting with their legs and not their back, or arranging their study area to avoid slouching—can help protect their spine during everyday activities.
Conclusion
By combining strengthening routines, healthy habits, and guidance from your healthcare provider, you’ll support your child’s journey to a stronger, pain-free back.
Finally, it is important to note that this document serves as an informational guide and should not replace professional medical advice. If you suspect that a child may have a Pars Defect or any other medical condition, it is recommended that you give us a call and schedule an appointment at one of our three offices – Dallas, Arlington, Flower Mound, Frisco, and McKinney, TX. At the Medical City Children’s and Spine Specialists Medical Practice, our doctors specialize in treating children and treating those with spine conditions that cause pain.
____________________
Citation: National Library of Medicine – Pars Defect
The medical content on this page has been carefully reviewed and approved for accuracy by the Medical City Children’s Orthopedics and Spine Specialists qualified healthcare professionals, including our board-certified physicians and Physician Assistants. Our team ensures that all information reflects the latest evidence-based practices and meets rigorous standards of medical accuracy, with oversight from our expert spine doctors to guarantee reliability for our patients.
Call 214-556-0590 to make an appointment.
Comprehensive services for children from birth through adolescence at five convenient locations: Arlington, Dallas, Frisco and McKinney.
