
SPLIT SPINAL CORD MALFORMATION
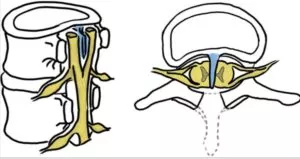
Split spinal cord malformation (SSCM) is a rare form of spinal dysraphism in which a mother gives birth to a baby with this splitting, or duplicated spinal cord. It may be characterized by complete or incomplete division of the spinal cord, resulting in two ‘hemicords.
If your child needs surgery or casting, our Fracture Care Clinic opens every day and you do not need an appointment. Surgery rooms get scheduled every morning, so your child receives the care and attention they need right away.
Split Spinal Cord Malformation
Split Spinal Cord Malformation, also known as Diastematomyelia, is a rare congenital condition that affects the spinal cord. The condition describes a spinal cord with two halves — separated by a bony or fibrous septum. This can cause a range of neurological symptoms, which may vary depending on the severity and location of the split.
Causes and Types of Split Spinal Cord Malformation
 The causes of SSCM are not fully understood, but there are several theories as to why it occurs. One theory suggests that SSCM is caused by a disruption in the development of the neural tube. This tube forms the brain and spinal cord during fetal development. Some believe the disruption could form from genetic mutations, environmental factors, or a combination of both. Another theory proposes that SSCM occurs because of abnormal vascular development. Therefore, leading to the formation of an abnormal blood vessel that compresses and splits the spinal cord.
The causes of SSCM are not fully understood, but there are several theories as to why it occurs. One theory suggests that SSCM is caused by a disruption in the development of the neural tube. This tube forms the brain and spinal cord during fetal development. Some believe the disruption could form from genetic mutations, environmental factors, or a combination of both. Another theory proposes that SSCM occurs because of abnormal vascular development. Therefore, leading to the formation of an abnormal blood vessel that compresses and splits the spinal cord.
Researchers have identified several genetic mutations that may increase the risk of SSCM. These include mutations in the genes that regulate neural tube development. Additionally, environmental factors such as maternal infections, exposure to certain toxins, and nutritional deficiencies have been linked to an increased risk of SSCM. It is important to note that SSCM is a congenital condition, which means it is present from birth. However, symptoms may not become apparent until later in life, depending on the severity and location of the split. Overall, the causes of SSCM are complex and multifactorial. Further research needs to fully understand the underlying mechanisms of this condition.
QUESTIONS AND ANSWERS
What is Diastematomyelia, and how did my child develop this condition?
Diastematomyelia is a congenital disorder characterized by the presence of a cleft or split in the spinal cord. This split can be associated with a bony spur or septum. The exact cause of Diastematomyelia is not always clear, but it is believed to result from abnormal embryonic development during the early stages of pregnancy. Genetic and environmental factors may contribute. The condition is typically present from birth and may be detected during infancy or childhood.
What are the treatment options for Diastematomyelia, and what is the prognosis for my child?
The treatment for Diastematomyelia depends on the severity of the condition and the presence of associated abnormalities. In some cases, surgical intervention may be recommended to address the split in the spinal cord and correct any associated issues. The prognosis varies depending on factors such as the extent of the malformation and the success of surgical interventions.
With appropriate medical care and management, many individuals with Diastematomyelia can lead relatively normal lives. However, the outcome can vary, and the healthcare team will provide more specific information based on the child’s individual case.
What kind of follow-up care and support does my child need after treatment?
Schedule an appointment and see a pediatric orthopedist quickly at Medical City Children’s Orthopedics and Spine Specialists.
Types
There are two main types of SSCM: Type I and Type II.
- Type I SSCM, also known as Diastematomyelia, occurs when the spinal cord gets split into two separate halves by a bony or fibrous septum. This septum can cause pressure on the spinal cord and can lead to neurological symptoms.
- Type II SSCM, also known as Diplomyelia, occurs when the spinal cord gets split into two separate halves, but with no septum between them. Instead, each half of the spinal cord becomes surrounded by its own dural sac, which can cause pressure on the spinal cord and lead to neurological symptoms.
In addition to these two main types, there are several subtypes of SSCM that have been identified. The identity of the subtypes become based on the location and severity of the split. These subtypes include dorsal, ventral, and lateral split malformations, as well as complete and incomplete forms of the condition.
Symptoms of Split Spinal Cord Malformation
The symptoms of Split Spinal Cord Malformation (SSCM) can vary depending on the severity and location of the split. In some cases, the patient may exhibit no symptoms at all. However, in other cases, the condition can cause a range of neurological problems.
Common symptoms of SSCM may include:
- Back pain: People with SSCM may experience chronic back pain due to pressure on the spinal cord.
- Muscle weakness: Depending on the location of the split, people with SSCM may experience muscle weakness in the legs or arms.
- Sensory changes: SSCM can cause sensory changes, such as numbness or tingling, in the affected areas of the body.
- Bladder and bowel problems: SSCM can affect bladder and bowel function, leading to incontinence or difficulty with urination and bowel movements.
- Scoliosis: Some people with SSCM may develop scoliosis, a curvature of the spine.
- Foot deformities: In some cases, SSCM can cause foot deformities, such as clubfoot or other abnormalities.
- Hydrocephalus: In rare cases, SSCM exists with hydrocephalus, a condition where there is an accumulation of fluid in the brain.
The severity of symptoms can vary between severe and none at all for individuals with SSCM. If you or a loved one are experiencing any of these symptoms, it is important to seek medical attention. Expert doctors like those at Medical City Children’s Orthopedics and Spine Specialists will test the patient to confirm SSCM and immediately devise a treatment plan.
Diagnosis of Split Spinal Cord Malformation
To diagnose Split Spinal Cord Malformation (SSCM), doctors may perform a variety of tests and exams. The diagnose will evaluate the patient’s symptoms and determine the location and severity of the split in the spinal cord.
Some of the diagnostic tests that diagnose SSCM include:
- Magnetic resonance imaging (MRI): This imaging test uses powerful magnets and radio waves to create detailed images of the spinal cord and surrounding tissues. An MRI can help identify the location and extent of the split in the spinal cord.
- Computed tomography (CT) scan: A CT scan can provide detailed images of the bones and soft tissues of the spine. The scan can help identify any abnormalities or malformations.
- Electromyography (EMG): This test measures the electrical activity of muscles. This test can help determine if there is any nerve damage or muscle weakness in the affected area.
- Spinal tap (lumbar puncture): A spinal tap can help rule out other conditions, such as infection or inflammation, that may cause the patient’s symptoms.
- Neurological exam: A doctor may perform a neurological exam to assess the patient’s reflexes, muscle strength, and sensation in the affected areas.
In some cases, doctors can diagnosis SSCM during a prenatal ultrasound or other imaging studies before birth. However, in other cases, doctors cannot diagnose the condition until later in life when symptoms appear.
It is important to seek medical attention if your child has any symptoms of SSCM. An accurate diagnosis is critical for developing an effective treatment plan.
Surgical and Non-Surgical Treatments for Split Spinal Cord Malformation
The treatment for Split Spinal Cord Malformation typically involves a combination of surgical and non-surgical interventions. It all depends on the severity and location of the split. Non-surgical treatments may include physical therapy to improve muscle strength and mobility. In addition, doctors may consider pain management techniques such as medications or nerve blocks . Surgical intervention may become necessary where the spinal cord split causes significant neurological symptoms or complications such as syringomyelia. The type of surgery performed will depend on the location and extent of the split. Of course the doctor will consider the individual’s overall health as well.
In some cases, surgery may involve removing the bony or fibrous septum that is dividing the spinal cord. However, in other cases it may involve fusing the two halves of the spinal cord together to restore normal function.
Prevention Measures and Recovery Time for Split Spinal Cord Malformation
As Split Spinal Cord Malformation is a congenital condition, there are no specific preventive measures that can avoid the condition. The recovery time for Split Spinal Cord Malformation will depend on the severity of the condition and the type of treatment received. In cases where non-surgical treatments are effective, individuals may resume normal activities relatively quickly. However, in cases where surgery is required, recovery time takes longer and may involve a period of physical therapy to regain strength and mobility.
In general, individuals with Split Spinal Cord Malformation may require ongoing monitoring and management of their symptoms, as the condition can cause progressive neurological complications over time.
Finally, our doctors at Medical City Children’s Orthopedics and Spine Specialists, with offices in Arlington, Dallas, Flower Mound, Frisco, and McKinney, TX, understand the importance of maintaining your child’s health. In addition, our experts and specialists have the training, knowledge, and experience required to take care of a split spinal cord malformation. If your child is born with this condition, don’t hesitate to call our office at 214-556-0590 to schedule an appointment at one of our five locations.
____________________
Footnote:
National Organization of Rare Diseases: Split Spinal Cord Malformation
Call 214-556-0590 to make an appointment.

