
PERTHES DISEASE
Perthes disease refers to a rare childhood condition that affects the hip joint. It occurs when the blood supply to the ball portion of the hip joint is temporarily interrupted. The weakened bone gradually loses its round shape. The body will restore the blood supply to the ball, and the ball heals. But if the ball is no longer round after it heals, it can cause pain and stiffness.
At the Medical City Children’s Orthopedics and Spine Specialists medical practice, our expert Hip Doctors and surgeons are dedicated to diagnosing and treating children with all types of medical conditions to ensure comprehensive care is tailored to each patient’s needs. We only specialize in children’s health, and we have undergone advanced training to do so. We treat minor and very major medical conditions with a compassionate approach, and our team cares for patients suffering from Perthes Disease.
“Some conditions need treatment early on while growth potential continues.”
Perthes Disease
 Perthes disease, a rare childhood condition, affects the hip joint. Also known as Legg-Calve-Perthes disease in honor of the team of doctors that first described the condition, it occurs in about 5.5 children per 100,000. The lifetime risk of developing Perthes disease equals 1 in 1200. Boys get the condition three to five times more affected than girls.
Perthes disease, a rare childhood condition, affects the hip joint. Also known as Legg-Calve-Perthes disease in honor of the team of doctors that first described the condition, it occurs in about 5.5 children per 100,000. The lifetime risk of developing Perthes disease equals 1 in 1200. Boys get the condition three to five times more affected than girls.
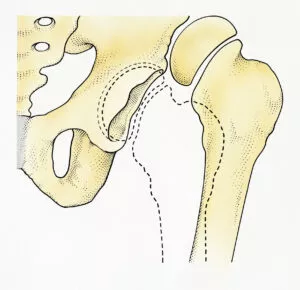
This condition, a form of osteochondritis, affects the hip. Normally, it develops as a unilateral condition. When bilateral Perthes disease occurs, the child should get evaluated for other conditions, such as multiple epiphyseal dysplasias. It develops by the cessation of blood flow to the head of the femur.
This happens when the artery of the ligamentum teres femoris becomes constricted or blocked too early. As a result of this disruption, the bone stops growing and starts to deteriorate. Later, healing occurs, and new blood vessels infiltrate the bone to remove the injured parts. This causes a loss of bone mass and femoral head.
Perthes disease becomes evident in children between the ages of four and eight, but the condition has been described in patients as young as two and as old as fifteen.
How Long Does Perthes Disease Last?
Perthes disease is not a quick, overnight occurrence. Instead, it unfolds in stages and can take several years to run its full course. Most children experience symptoms and changes in the hip for a period of two to four years. In some cases, the process may extend even longer, depending on the child’s age at diagnosis and the progression of bone healing. This drawn-out timeline is important because it impacts both treatment approaches and the final outcome for the hip joint.
QUESTIONS AND ANSWERS
What is Perthes disease, and what caused it in my child?
Perthes disease is a childhood condition that affects the blood supply to the ball-shaped head of the femur (thigh bone) in the hip joint. The reduced blood flow can lead to the death of a segment of the bone, causing it to collapse. The exact cause is often unknown, but it is believed to be related to a combination of genetic and environmental factors. There is no evidence to suggest that specific activities or behaviors cause Perthes disease.
What is the recommended treatment for Perthes disease, and what is the expected outcome?
The treatment approach for Perthes disease depends on various factors, including the child’s age, the extent of involvement, and the stage of the disease. Common treatment options include rest, activity modification, physical therapy, and sometimes bracing or casting. In more severe cases, surgical interventions may be considered.
The goal of treatment is to maintain the round shape of the femoral head and improve the function of the hip joint. The outlook varies for each child, but with appropriate treatment, many children with Perthes disease go on to have normal hip function as they grow.
How can we support our child during the treatment and recovery process?
Parents often want to know how they can best support their child during the challenging period of Perthes disease. This involves adhering to the treatment plan prescribed by the healthcare provider, which may include restrictions on certain activities, ensuring the child wears any recommended braces or casts, and attending regular follow-up appointments. Encouraging the child to engage in approved low-impact activities and maintaining a positive and supportive environment can also contribute to their well-being. It’s essential for parents to communicate openly with the healthcare team, ask questions, and stay actively involved in their child’s care.
It’s important to note that the information provided here is general, and specific details about Perthes disease and its management should be discussed with the child’s healthcare provider. Each case is unique, and the doctor will tailor the treatment plan based on the individual characteristics of the condition.
We specialize in children, and our practice only sees children. Call for an appointment.
Stages of Perthes’ Disease
Perthes disease unfolds in a sequence of distinct stages, each with its hallmark features and implications for the growing hip.
- Initial (Necrotic) Stage: This opening stage marks the interruption of blood flow to the femoral head. With the bone starved of nutrients, cells within the ball of the hip die. Children may begin to walk differently, often with a noticeable limp, as inflammation sets in. This phase can last several months.
- Fragmentation Stage: Over the course of one to two years, the body starts breaking down the damaged bone and replacing it with soft, new bone. This is a delicate time: the femoral head becomes weak and vulnerable to flattening. On an X-ray, it may appear as though the bone is in fragments or “pieces,” and the hip is at its most unstable.
- Re-ossification Stage: During this prolonged phase—often the longest—the body gradually forms new, denser, and stronger bone in the femoral head. Restoration is slow, spanning several years, as the bone regains its structure and shape.
- Healed (Remodeling) Stage: Finally, the bone regrowth concludes. The femoral head settles into its permanent shape, which may or may not return to perfect roundness. The eventual contour depends on factors such as the degree of earlier damage and the child’s age when the disease began, since younger children have more time for the bone to reshape as they grow.
Perthes Disease Causes
Today, doctors do not know the cause of Perthes disease.
Some studies link the disease to tobacco smoke exposure and genetics. But the association remains unclear. Some studies suggest a genetic origin because children whose parents had the condition possess a slightly greater risk. Also, researchers do not know if a true genetic link exists or if the cause relates to a common environmental factor. More research will help uncover and document the true cause of Perthes disease.
Perthes Disease Symptoms
The most recognizable symptom of Perthes disease occurs when observing the child walking or running. For instance, a child who walks or runs awkwardly should get evaluated for Perthes disease. Thus, the change in the child’s way of walking or running becomes obvious while participating in sports activities.
One of the earliest signs parents might notice is a limp or a peculiar running style, especially during active play or sports. This change is often due to irritation within the hip joint. The symptoms can be subtle at first—sometimes just a slight limp that comes and goes, or complaints of soreness after a busy day.
Other symptoms that might be present:
- Pain in the hip
- Pain in the knee
- Limping
- Pain in the leg
- Pain in the thigh
- Limited motion
- Pain in the groin
- Awkward style of walking
- Awkward style of running
- Painful muscle spasms in the hip or leg
- Change in a child’s walking
- Change in a child’s running
- Pain that worsens with activity and goes away with rest
It’s important to note that pain from Perthes disease isn’t always felt in the hip. Children may report pain in the thigh or even the knee—this is known as referred pain and can sometimes make diagnosis tricky. Painful muscle spasms in the hip or leg may also occur as a result of irritation around the joint. These symptoms might not be constant. In most cases, they come and go over several weeks before caregivers decide to seek medical attention. Depending on your child’s activity level, you might notice these issues flare up during periods of increased activity and improve with rest.
Recognizing these early changes can help ensure prompt evaluation and treatment, giving your child the best chance for healthy hip development.
What is referred to as pain in the context of Perthes disease?
Referred pain happens when discomfort from the hip joint, where Perthes disease is active, is felt in other areas like the thigh, knee, or groin. In children, it’s common for pain to show up not just at the hip but also in the knee or along the leg, even though the source of the problem is actually at the hip. This can sometimes make it harder to recognize Perthes disease right away, since the pain isn’t always at the site of the real issue. If your child complains of knee or thigh pain, especially with no clear injury, it’s important to consider the possibility of hip involvement and have them evaluated by a healthcare provider.
Doctor’s Consultation
At your child’s initial exam with your Orthopedic Specialist, the doctor will evaluate your child’s gait and make a list of the current symptoms your child displays. Coupling it with a thorough history of your child’s health, a physical examination, and possibly ordering several diagnostic tests. These additional tests will help complete an accurate diagnosis for your child. Your doctor will want to know the child’s age when symptoms started, and how they progress. The doctor will ask for a list of any treatments received. Finally, your doctor will want to know about any presence of family history. He will also ask if there are any similar orthopedic conditions, among other details about your child.
Diagnosing Perthes Disease
A doctor diagnoses Perthes disease, or Legg-Calvé-Perthes syndrome, using clinical evaluation, patient history, and imaging studies. The doctor begins by asking about limping, hip or knee pain, reduced motion, and any recent trauma or family history. Although causes are often idiopathic, understanding symptoms and patterns helps guide further evaluation. During the physical exam, the doctor observes gait and checks for limited hip motion, especially abduction and internal rotation. The doctor also looks for muscle atrophy or leg length differences that may signal chronic problems.
These symptoms typically appear in children between the ages of 4 and 10, with boys more commonly affected than girls.
To confirm the diagnosis, the doctor uses imaging. X-rays usually come first and may show flattening or fragmentation of the femoral head. Early-stage disease may appear normal on X-rays, requiring follow-up imaging. If X-rays don’t confirm the diagnosis, the doctor may order an MRI.
MRI scans show detailed views of cartilage, bone, and early signs of blood supply loss. In some cases, a bone scan helps evaluate blood flow to the femoral head. The doctor may also order blood tests to rule out infections like septic arthritis. To exclude slipped capital femoral epiphysis, the doctor uses additional imaging. This thorough, step-by-step approach allows accurate diagnosis and guides the right treatment plan.
What is an Arthrogram and Why is it Needed?
An arthrogram is a special imaging procedure that your doctor may recommend as part of your child’s evaluation or treatment. To perform an arthrogram, the doctor injects a small amount of dye directly into the hip joint. This dye helps provide a much clearer picture of the femoral head (the ball at the top of the thigh bone) on X-ray images.
The main reason for using an arthrogram is to get a detailed look at the shape and placement of the femoral head inside the hip joint. This is especially important if your child’s doctor needs to assess the degree of any changes or deformity in the bone. The images from an arthrogram can help the care team plan any procedures more precisely and ensure that the hip joint is positioned properly throughout treatment. This extra level of detail allows for a more tailored, effective approach, ultimately helping to protect your child’s joint health as they heal.
Perthes Disease Treatment
The goals of treatment for Perthes’ disease are threefold:
- Stop pain
- Protect the femoral head shape
- Restore the normal range of hip movements
Without treatment, the head of the femur becomes permanently deformed. The child becomes more likely to develop hip problems like arthritis as they age into adulthood.
There are many treatment options for Perthes disease. The option chosen for your child will rely on several different indicators, for instance:
- Child’s age: The younger the child, the better. Diagnosing and treating younger children provides a much better chance of healing. Children who are six and below are usually able to grow new healthy bones to replace the injured ones.
- The stage of the disease: The treatment options when diagnosed earlier can utilize non-surgical treatments, hopefully without surgery. When the disease is diagnosed later in life, it is more likely that the child will require a surgical intervention.
- The degree of damage to the femoral head: If the femoral head appears more than 50% damaged, it will likely require surgery. Without intervention, the likelihood of the bone healing without a deformity is low. This means that the doctor may consider surgical measures to resize the bone. This resizing will help reshape the bone to the intended size and reposition it.
There is a range of surgical and nonsurgical procedures for treating Perthes’ disease, depending on your diagnosis.
Perthes Disease Non-Surgical Treatments
Normally, non-surgical treatments are commonly used for younger children with early disease and minimal damage to the femoral head. Depending on your doctor’s assessment and diagnosis, your child will receive a treatment plan. Below are some non-surgical treatments your doctor might adopt in the treatment of Perthes disease.
Observation
For this reason, with young children, early-stage disease, and minimal damage to the femoral head, observation is the treatment. One of the non-surgical treatments is simply to observe the bones and the child’s symptoms. During this process, your doctor will order a series of X-rays to monitor the progress of the condition of the bones. As the disease runs its course and as long as the bone is healing properly and the symptoms are relieved, no further treatments will be required, except for periodic checkups.
Medication
Medicine offers another treatment and relieves pain. Pain in Perthes disease occurs from inflammation of the hip joint. To relieve this pain, your doctor can prescribe anti-inflammatory, pain-relieving medication. One of the drugs commonly prescribed for this condition is Ibuprofen. Your doctor can place your child on ibuprofen for many weeks while monitoring their progress. Changing the dose or stopping the drug can be decided based on the condition.
Protecting the joint
In order to facilitate healing and prevent the condition from getting worse, your doctor will want to protect the joint. Protecting the joint involves two main activities:
- Limiting activity
- The use of walking aids.
Your doctor may advise your child to avoid running, jumping, vigorous walking, or any other activities that can strain the joint. Your doctor may also recommend walking aids. These may include crutches or a walker to reduce load-bearing on the affected hip and facilitate healing.
Physiotherapy (Physical therapy)
Perthes disease causes stiffness and limits the range of motion around the hip joint. Doctors aim to restore normal movement in the hip. Physical therapy plays a key role in achieving this goal. The physical therapist teaches exercises that improve hip motion in both outward and inward directions.
These exercises strengthen the muscles that move the hip and support normal joint function.
Regular physiotherapy focuses on improving hip abduction and internal rotation. Abduction means moving the leg away from the body. Internal rotation involves turning the leg inward. Children with Perthes disease often struggle with these movements. Targeted exercises help prevent long-term stiffness. Your physical therapist may recommend these common exercises:
- Hip abduction exercise: Your child lies on their back with knees bent and feet flat. They gently push their knees apart, then squeeze them together. A caregiver can assist by placing their hands on the knees to increase the motion range.
- Hip rotation exercise: Your child lies flat with legs straight. A caregiver rolls the leg inward and outward gently. This helps maintain flexibility and reduce hip stiffness.
Perform these exercises daily with caregiver support. Your physical therapist will demonstrate and guide you on safe home practice.
Continue physiotherapy throughout healing to maintain joint mobility and function. Regular exercise helps the hip recover and restores natural movement.
Casting and Bracing
Casting and bracing are other non-surgical treatment options that can help your child. This option is usually adopted if the X-rays show the formation of a deformity or the range of motion is limited. Using special casts known as Petrie casts, your doctor will immobilize the hip in the best position for healing. Petrie casts are specialized casts shaped like the letter “A”.
Petrie casts are usually applied in the operating room. This allows your doctor to conduct several special X-rays called Anagrams, which help to visualize the head of the femur in the correct position. It also allows him to carry out any minor procedures required, such as a Tenotom, where a small incision in the muscle will relieve tightness.
Tenotomy procedure
In some cases, the adductor longus muscle in the groin can be very tight and prevent the hip from rotating into the proper position. When this happens, your doctor may recommend a tenotomy—a minor surgical procedure to release the tightness. During this quick procedure, a thin instrument is used to make a small incision in the muscle, allowing better positioning of the hip before the Petrie casts are applied.
Doctors will implement casts for up to six weeks at a time. Based on the progression of the disease, doctors will apply intermittent casting. After casting, your child will require physical therapy to regain their range of movement.
Surgical Treatments
In older children with advanced Perthes disease and more than 50% damage to the femoral head, the treatment option includes surgery. So, surgery is recommended when the non-surgical methods fail.
The most common type of surgery is an osteotomy. During an osteotomy, your doctor will cut the bone and reposition it to make sure the femoral head fits within the socket. Then the bone will be held in place with screws and plates until it heals. Following the surgery, the patient gets a cast to aid proper healing. Physical therapy gets scheduled when the cast is removed to build your child’s muscles and help with walking correctly.
After the cast is removed:
- Your child will need physical therapy to restore muscle strength and range of motion.
- Crutches or a walker may be necessary to reduce weight-bearing on the affected hip while the bone continues to heal.
- Your child’s doctor will monitor the hip’s recovery with follow-up X-rays to ensure proper healing and alignment through the final stages.
These steps are essential to ensure optimal recovery and help your child regain normal hip function after surgery.
Prognosis/Outcome
Finally, the prognosis for Perthes disease remains good. Children who are younger than six years old have the best prognosis because their bones have enough time to easily revascularize and remodel. With proper treatment, most children are able to grow into adulthood without any further concerns. Also, the prognosis depends on how well the head of the femur fits into the acetabulum. This, in turn, depends on the shape of the femoral head and the congruence of the hip. If the femoral head fits well, then doctors expect a full recovery. If it does not, then the child might develop problems such as arthritis and Coxa Magna as they age.
Why Choose Medical City Children’s Orthopedics and Spine Specialists
The Medical City Children’s Orthopedics and Spine Specialists doctors only treat children. Our doctors at Medical City Children’s Orthopedics and Spine Specialists are located in five convenient locations: Dallas, Arlington, Flower Mound, Frisco, and McKinney, TX, for families in the Dallas and Fort Worth area. Selecting a pediatric orthopedic doctor for your child who knows how to treat Perthes Disease is a crucial decision that requires careful consideration. Doctors Shyam Kishan, Richard Hostin, and Kathryn Wiesman have spent years studying children’s health and have devoted their lives to treating them. If your child has Perthes Disease, please call our office for an appointment.
_____________________
Citation: Orthoinfo – Perthes Disease
The medical content on this page has been carefully reviewed and approved for accuracy by the Medical City Children’s Orthopedics and Spine Specialists qualified healthcare professionals, including our board-certified physicians and Physician Assistants. Our team ensures that all information reflects the latest evidence-based practices and meets rigorous standards of medical accuracy, with oversight from our expert spine doctors to guarantee reliability for our patients.
Our physicians at Medical City Children’s Orthopedic and Spine Specialists have experience and expertise in the treatment of Perthes Disease. You will see specialists, and should the doctors recommend surgery, you will get access to an operating room right away. Our board-certified physicians specialize in the treatment of children and adolescents. Give your child the very best care and attention they deserve.
Call 214-556-0590 to make an appointment.
Comprehensive services for children from birth through adolescence at
four convenient locations: Arlington, Dallas, Flower Mound, Frisco and McKinney.

