Sinding-Larsen-Johansson Syndrome:
 The Sinding-Larsen-Johansson syndrome is short-term damage to the knee’s growth plate. It mostly affects children and teenagers aged 10 to 14 and is usually caused by overuse as a result of sports participation. Rest, ice, and over-the-counter drugs are generally enough to heal it. While their tendon heals, children should avoid sports or strenuous physical activity.
The Sinding-Larsen-Johansson syndrome is short-term damage to the knee’s growth plate. It mostly affects children and teenagers aged 10 to 14 and is usually caused by overuse as a result of sports participation. Rest, ice, and over-the-counter drugs are generally enough to heal it. While their tendon heals, children should avoid sports or strenuous physical activity.
What is Sinding-Larsen-Johansson Syndrome?
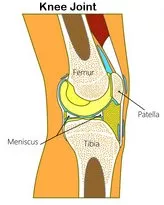
Sinding-Larsen-Johansson syndrome (SLJ) is a growth plate injury where your kneecap (patella) links to your patellar tendon, which connects your kneecap to your shin bone (tibia). SLJ is a tendon injury that occurs when the tendon connects to the kneecap (the inferior pole of your patella). It primarily affects youngsters aged 10 to 14 who participate in sports or are physically active. Your patellar tendon joins your kneecap to your shin like a thick rubber band. It is responsible for holding the bones together and allowing them to move correctly. When children strain their thigh muscles, they produce Sinding-Larsen-Johansson syndrome, which is caused by recurrent tension and pressure on the patellar tendon (quadriceps). Any repeated motion might create the overuse that leads to SLJ, including:
- Any activity or sport that requires children to exert a lot of effort with their legs and knees on a regular basis.
What Makes Osgood-Schlatter Disease Different from Sinding-Larsen-Johansson Syndrome?
Many of the origins, symptoms, and treatments for Sinding-Larsen-Johansson syndrome and Osgood-Schlatter Disease are remarkably similar. Both disorders pertain to injuries to the patellar tendons in children and teenagers. The key distinction is the injury to which section of the patellar tendon. Sinding-Larsen-Johansson syndrome is a tendon injury at the top (the proximal end). The bottom (distal end) of the tendon is affected by Osgood-Schlatter disease. Young individuals with SLJ destroy the tendon where it exits the kneecap, whereas those with Osgood-Schlatter disease damage it where it departs the shin.
Doctors know that The distinction between Sinding-Larsen-Johansson syndrome and Osgood-Schlatter disease requires expertise in both conditions. That resemblance, on the other hand, helps because doctors will ease your child’s symptoms with the same therapies since they’re both caused by overuse — commonly from sports — and the most frequent treatments involve rest and medicine to minimize swelling. Your doctor will explain the details of what’s causing your child’s pain and why it’s SLJ or Osgood-Schlatter disease.
Sinding-Larsen-Johansson Syndrome is a Condition that Affects People of all Ages
Children and teenagers between the ages of 10 and 14 are affected by Sinding-Larsen-Johansson syndrome. Cerebral palsy patients are more likely to develop SLJ, according to studies. Because of how children’s bodies grow and change, the age range is rather narrow. The growth plate at the top of their shinbone is particularly active and susceptible to injuries between the ages of 10 and 14. Growth spurts, which occur when a child’s bones, muscles, and tendons all change at the same time, can put their knees under additional strain.
Sinding-Larsen-Johansson Syndrome in Adults
Adults can suffer from Sinding-Larsen-Johansson syndrome, although it is extremely unusual. In reality, if you are above 15 years old and have symptoms identical to SLJ, you are most certainly suffering from another illness known as “jumper’s knee.” Knee pain in adults emanates from a number of things. If you feel any new discomfort, especially after any strenuous physical activity, contact your healthcare practitioner.
What is the Prevalence of Sinding-Larsen-Johansson Syndrome?
Sinding-Larsen-Johansson syndrome affects a large number of people. It’s a common source of knee discomfort in teenagers.
What is the Impact of Sinding-Larsen-Johansson Syndrome on my Child’s Body?
Although excruciatingly painful, Sinding-Larsen-Johansson syndrome does not cause long-term effects on your child’s health or ability to resume their favorite activities. They’ll need to relax and avoid the activity or sport that caused SLJ for a few months, but after their patellar tendon recovers, they shouldn’t have any long-term effects.
Sinding-Larsen-Johansson Syndrome Manifests Itself in a Variety of Ways:
The following are the most prevalent symptoms of Sinding-Larsen-Johansson syndrome:
- Sharp discomfort just above the shin on the bottom of your child’s knee.
- Tenderness in the vicinity of their knee.
- They are having trouble bending their knee as far as they can normally.
Sinding-Larsen-Johansson Syndrome is Caused by a Combination of Factors
Overuse of the patellar tendon causes Sinding-Larsen-Johansson syndrome. It most typically affects children and teenagers who participate in sports, as it does with other types of osteochondritis. When your child uses excessive force — for example, when sprinting fast or kicking a soccer ball — they might injure their patellar tendon in a little, imperceptible way. These “micro traumas” can lead to SLJ, which is characterized by pain and edema.
What are the Symptoms of Sinding-Larsen-Johansson Syndrome?
The doctor will examine your child’s knee and shin, and your child will respond to questions about when he or she first experienced the discomfort. Your kid will almost certainly undergo imaging testing in order to confirm Sinding-Larsen-Johansson syndrome and rule out other illnesses or traumas.
Sinding-Larsen-Johansson Syndrome Tests
The diagnosis of Sinding-Larsen-Johansson syndrome uses a variety of imaging techniques, including:
X-rays: If your child’s kneecap, shin, or other bones are shattered, an X-ray will reveal it (fractured). An X-ray will check for a stress fracture in the shin, which is very prevalent among athletes.
Magnetic Resonance Imaging (MRI): An MRI will provide a detailed image of your child’s knee, as well as the surrounding area. If the patellar tendon has swollen as a consequence of the damage, the MRI will show this.
Ultrasound: The blood flow through the muscles and connective tissue surrounding your child’s knee will be visualized via an ultrasound.
How is Sinding-Larsen-Johansson Syndrome Treated?
Sinding-Larsen-Johansson syndrome is most commonly treated with rest and quadriceps stretching. While the patellar tendon heals, your kid should refrain from participating in the sport(s) that caused the injury. Most youngsters need to take a break from athletics for a few weeks to a few months. The length of time your child will need to rest is determined by the severity of the original injury. While they recuperate, your child may substitute their original sport with other, less physically demanding activities (such as swimming). In the near term, you can ease discomfort and reduce inflammation by icing your child’s knee and using over-the-counter NSAIDs.
Sinding-Larsen-Johansson Syndrome Surgery
Sinding-Larsen-Johansson syndrome is very unlikely to require surgery for your child. Discuss your child’s treatment choices with your doctor. Even in the most severe cases, your doctor would most likely recommend less intrusive therapies like physical therapy before recommending surgery for a kid or teen’s SLJ. Adults with SLJ may require knee surgery to repair their patellar tendons in some circumstances.
What Medications/Treatments Are Used?
Over-the-counter Sinding-Larsen-Johansson syndrome is commonly treated with Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen. Inflammation and edema are also reduced by NSAIDs. To relieve pain, your kid can take them as advised, but talk to your doctor before starting, stopping, or modifying any regular prescription usage. Without your provider’s permission, your kid should not take NSAIDs for more than 10 days in a row.
Complications/Side Effects of the Treatment
NSAIDs have a long list of potential adverse effects, including:
- Stomach pain.
- Bowel complications.
How Soon will my Child Feel Better Following Treatment?
Your youngster should feel better within an hour of starting to take the NSAIDs. The same is true when it comes to icing their knee. Although the pain alleviation stops, it does not imply that your child’s patellar tendon has healed. The most crucial element of your child’s treatment is resting and avoiding the activities that triggered their Sinding-Larsen-Johansson syndrome. Make sure you stick to the plan your healthcare practitioner offers you. Based on your child’s individual instance of Sinding-Larsen-Johansson syndrome, they’ll tell you how long it will take for them to feel better.
What can I do to Avoid Developing Sinding-Larsen-Johansson Syndrome?
Stretching the quadriceps (thigh muscles) on a daily basis is the greatest strategy to avoid Sinding-Larsen-Johansson syndrome. The less strain placed on your child’s tendons, the more flexible his or her legs are. To alleviate stress on the patellar tendon, it’s essential to adopt a few preventive measures, such as:
- Stretching before and after sports participation.
- Stopping and resting.
- It’s not the right thing to “play through the pain.”
What can I do to Lower my Child’s Chances of Developing Sinding-Larsen-Johansson Syndrome?
You may assist your youngster in preventing patellar tendon injury before it develops. Making ensuring kids have enough time to relax and heal between sports seasons is one of the greatest methods to do so. Sinding-Larsen-Johansson syndrome affects more children and teenagers than ever before. The most common reason is year-round participation in or training for a single sport. As more children focus on a single sport or activity, their bodies do not have the time to relax and recuperate. To lower their risk of all injuries, including SLJ, children, and teenagers should avoid specializing in one sport until they are in their late teens.
When Should I Schedule a Visit with a Doctor?
If your kid develops new discomfort in their knee, especially if it’s accompanied by swelling, you should take your child to a pediatric orthopedic doctor. The doctors at Medical City Children’s Orthopedics and Spine Specialists only treat children. As such, our knowledge, skills, and abilities regarding children’s illnesses and conditions are praised by other doctors in the Dallas and Fort Worth Metroplex. We urge you to call our office if you are concerned about your child’s health. We have convenient offices in Dallas, Arlington, Frisco, and McKinney, TX where we will see your child as quickly as possible.
____________________
American Medical Society for Sports Medicine: Sinding-Larsen-Johansson Syndrome

Recent Comments